


In the midst of this viral outbreak, we are all moving forward together and attempting to do what generations of human history have shown we do well – ADAPT. Dynamic change is the new normal, and for healthcare providers, it is happening hour to hour.
It’s a crisis of astronomical proportions, and while the CDC, WHO, and other academic societies are keeping us apprised with up-to-date clinical care information, additional concerns still remain. Workplace concerns have escalated everywhere, and healthcare is no exception. In addition to patient care, you are dealing with changing protocols, disruptions in routine, personnel management, personal wellness, and lack of communication.
At the same time, many are turning to you to be a strong leader. This may seem overwhelming. How do you navigate this role in this time of crisis?
In listening to several healthcare providers voice their concerns, I have consolidated the most common issues and provided some coping strategies for you to consider.
“I am confused as to how to be an effective provider.”
You have the education and training to qualify you to provide care, but this is a new virus that is increasing at an exponential rate. Guidance is unclear and rapidly changing. You have a right to feel vulnerable, exposed, and frustrated.
Seek guidance. Look to the experience of other providers. Remain open-minded and willing to change decisions quickly based on the situation. Remember that you do not need to make decisions alone. Try to focus discussions in team huddles. Try turning to peers and leaders in the institution and in your field.
“How do I reduce patient panic?”
Patients with conditions and disease states other than the coronavirus continue to arrive at clinics and hospitals nationally. Resources in healthcare are limited and so panic is expected.
Start with your internal teams to plan how you are going to prioritize patients, which remote workflows you are going to implement, and then how you will communicate that information to others.
Devise a plan on how to prioritize patients. Major medical centers have already announced plans to cancel elective procedures and surgeries. Consider postponing well visits and annual physicals. What are other patient visit types that can be scheduled out by 4, 8, or 12 weeks? This way if you have less ancillary support to provide care and need open slots in the schedule for the very ill, you have allotted the necessary time.
Remote workflows, or telehealth, offer a solution to help maintaining human contact in the time of strict social distancing. Workflows can be designed for live video-conferencing, transmission of still images, email, and phone calls to help with patient screening and triage. Free services such as Doxy Me are available to providers to implement for clinical workflow. Telehealth is a shift for many healthcare providers, but virtual care is becoming increasingly effective in our current environment.
Once your plans are in place, (and be open to changes as they will occur), it is critical to COMMUNICATE, COMMUNICATE, COMMUNICATE! Be sure that you and your care team have coordinated messaging. Get the word out via posters in patient care areas, emails out to all patients, recorded messaging on your phone lines, and posting video messages on all patient portals. Ease patient anxiety by helping them understand your plans and communicating them out in various forums.
“Some members of my staff are panicking.”
As a healthcare provider, you are a leader. Whether you lead a care team or certain care related individuals, people will turn to you for guidance, especially as they are encountering their own professional and personal challenges caused with the growing coronavirus pandemic. Cycles of emotions of anxiety, anger, and nervousness are expected.
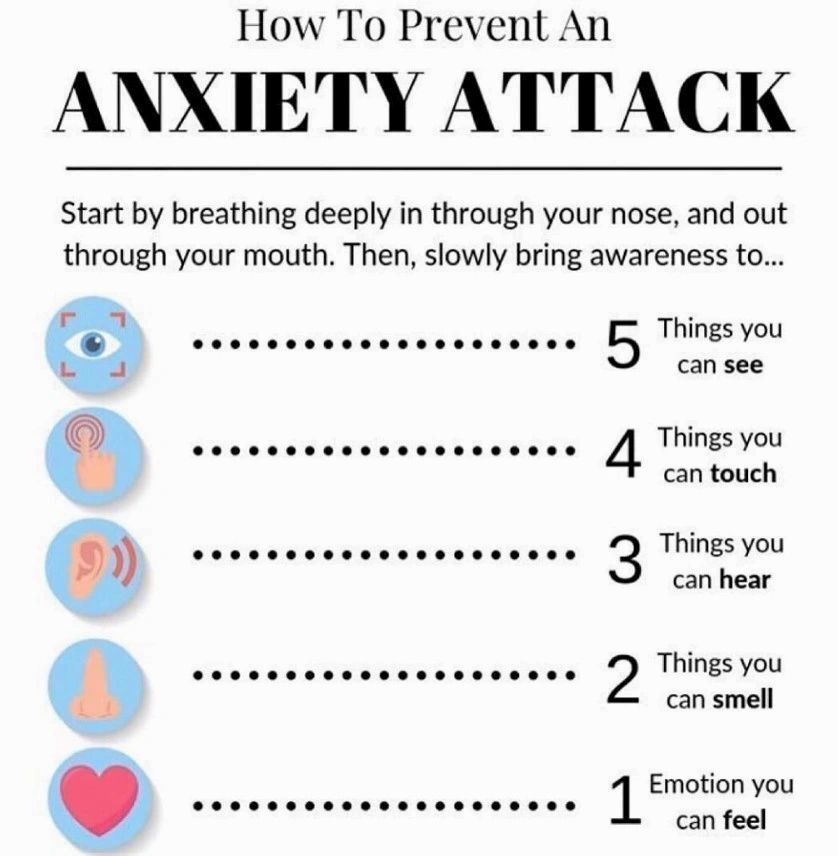
Before discussion, try starting with a quick mindfulness exercise to calm the nerves and manage anxiety. Psychologist Reena B. Patel, LEP, BCBA, recommends practicing “grounding” through a 5 step approach – breathe deeply through the nose and out of your mouth. Then slowly bring awareness to 5 things you can see, 4 things you can touch, 3 things you can hear, 2 things you can smell, 1 emotion you can feel.
After grounding, the goal is to get to the source of the panic – identify the specific concerns and address them individually. Is the staff being asked to reduce hours and/or pay? Review your institutional policies and discuss strategies with human resources to help. Are they worried about having to accommodate children whose schools have temporarily closed? Review what flexible accommodations can be made through scheduling. Whatever the issue, show empathy. You may not have all the answers, but good listening and understanding will help the staff arrive at options that will work for them.
“I have a fear for my own personal health.”
Your fear is real and justified. Being at the frontlines and having multiple patient contact, following the rules of social distancing are likely not possible in your profession. Try to focus your attention on taking action steps to mitigate your fears by examining the source of the unease.
First and foremost, keep up to date with the guidelines published by the CDC on how healthcare providers can protect themselves found here: https://www.cdc.gov/coronavirus/2019-ncov/hcp/caring-for-patients.html
Secondly, adhere to guidelines and make sure your team is doing so as well. Be clear about your concerns and provide options for possible solutions or be honest if you have exhausted your own options. Speak up about your fears and concerns with the leadership in your organization. If you don’t, they will assume you are doing fine and move on ahead. Lead by example. Be accountable and make others accountable.
Thirdly, explore options to reduce exposure through new clinical workflows. This includes changes in patient triage so for example, changing clinic times to have well patients in the morning and sicker patients in the afternoon. Additionally, review virtual platforms for telehealth and use them to conduct pre-visit screening (as mentioned above).
In summary:
You went into your profession understanding the impact you make on patients and knowing that, while you can’t take care of everyone, you will provide the best care you can for those under your watch. To be an effective healthcare provider, your practice patterns are going to change during this time of crisis. Understand this and give yourself the grace to adapt. And for any non-healthcare providers that are reading this – don’t just provide support, but also be a voice for our healthcare providers to ensure their concerns are being heard. Acknowledge concerns around infection control guidance and equipment and help provide solutions. Recognize the efforts of our healthcare providers.
If you have other concerns that you wish to discuss, feel free to reach out to me.
Aashi Arora, MHA, iRISE Executive Coaching
Contact: aashi@iriseexecutivecoaching.com
 Preparing to Step Into CEO Roles
May 30, 2023
Preparing to Step Into CEO Roles
May 30, 2023
 Tackle Imposter Syndrome by Prioritizing This Relationship
May 12, 2023
Tackle Imposter Syndrome by Prioritizing This Relationship
May 12, 2023
 How Do You Know It’s Imposter Syndrome?
Mar 08, 2023
How Do You Know It’s Imposter Syndrome?
Mar 08, 2023
 Imposter Syndrome During a Job Transition
Jan 20, 2023
Imposter Syndrome During a Job Transition
Jan 20, 2023
 4 Strategies for A Successful Interview
Oct 19, 2022
4 Strategies for A Successful Interview
Oct 19, 2022
Please subscribe to receive a pdf of 15 Ways to Tackle Imposter Syndrome
